Practice Matters
Mitigating Burnout: Transition to a Condensed Workweek for Advanced Practice Providers in Infectious Diseases
Shannon Holloway, PA-C, Kelly McConn, Pa-C, Roy Borchardt, PA-C, PhD, Victor E. Mulanovich, MD, and Javier A. Adachi, MD
From The University of Texas MD Anderson Cancer Center, Houston, Texas
Correspondence to: Shannon Holloway, PA-C, 1515 Holcombe Blvd, Houston, TX 77030
E-mail: sholloway@mdanderson.org
J Adv Pract Oncol 2023;14(7):639–643 |
https://doi.org/10.6004/jadpro.2023.14.7.8 |
© 2023 BroadcastMed LLC

 ABSTRACT
ABSTRACT
Burnout among health-care workers is highly prevalent and profoundly impacts the quality of patient care. In addition to affecting patient safety, burnout results in higher staff turnover, revenue deficits due to decreased productivity, financial risk, and diminished organization viability because of the impact on quality of care, patient satisfaction, and safety. Culmination of external and internal stressors in health-care worker populations is associated with a higher probability of burnout and workers who reported perceived low workplace flexibility. In addition, workplace flexibility is associated with reduced odds of experiencing burnout. Workplace flexibility plays a critical role in potentially reducing the occurrence of burnout in the health-care worker population. Individually focused solutions are important to mitigate burnout, however, comprehensive organizational change ensures durable and sustainable solutions. There is a correlation between a positive employee outlook and reduced stress when there is a perceived level of control over one’s work schedule. The goal of this article is to showcase the process of a successful implementation of a condensed work schedule for an advanced practice provider workforce in infectious diseases in response to burnout and workload shifts. This chronicles the steps of design, rationale, procuring buy-in by stakeholders, and operational implementation of the new schedules. Advanced practice provider satisfaction and burnout were measured by periodic surveys at timepoints along the way.
ARTICLE
Advanced practice providers (APPs) are an integral part of the health-care delivery system in the United States. They offer a cost-effective means of improving efficiency while maintaining high-quality patient care (American Association of Medical Colleges, 2021; Morgan et al., 2019). Advanced practice providers provide a multitude of contributions to health-care teams, which cannot be fully captured in productivity reporting of revenue and billing (Kuriakose et al., 2022).
As the utilization of APPs has increased across health-care settings, the level of burnout among APPs has increased as well. The World Health Organization (WHO) defines burnout as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: feelings of energy depletion or exhaustion; increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; and reduced professional efficacy” (WHO, 2019). Work-related burnout can lead to poorer physical health, higher risk of mental illness, low morale, incivility, poor job performance, errors, absenteeism, and turnover (Maslach, 2017). The COVID-19 pandemic exacerbated an already increasing level of burnout among health-care workers, as many APPs continued to work on the front lines of the pandemic under exceptionally heightened stress (Maunder et al., 2022).
Benefits of Workplace Flexibility
Increased workplace flexibility has been reported to mitigate burnout among health-care workers (Maunder et al., 2022). A recent report highlights the largest-scale trial to date was initiated in June 2021 in Britain, in which 61 companies with a total of 2,900 employees participated in a 4-day workweek trial. There were favorable results for the employees, reporting decreased burnout, decreased stress, and increased job satisfaction than was reported prior to starting the trial. There were also favorable results reported by the companies, with increased employee productivity and a growth in revenue reported by 47 companies. Ninety-two percent (56 of the 61 companies) stated that they would continue the new schedule, and 30% (18 companies) stated they had already adopted it as a permanent change (Barnell, 2023).
The transition to a condensed workweek for the authors took place within one department at a large academic cancer institution that employs over 1,100 APPs. The Infectious Diseases (ID) department APP group comprises 17 physician assistants and nurse practitioners who practice on busy inpatient services, as well as cover one outpatient clinic position. At the start of the pandemic, many medical practices transitioned to telemedicine in order to maintain social distancing and reduce the spread of COVID-19. Throughout the pandemic, the ID department continued to practice direct patient care on site, with a few telemedicine encounters as an exception.
For our group, as with inpatient care providers around the world, there was an unavoidable and exponential increase in work-related stress (Maunder et al., 2022). Not only was our group involved in the treatment of the expected highly complex infections in the immunocompromised patient population, but we were also involved in the care of all admitted COVID-19 patients at the institution. The added work-related stress was compounding the personal psychological stress of the pandemic, which has an inverse effect on self-efficacy (Maunder et al., 2022). During this period of mounting stress, the ID department also needed to implement higher weekend APP staffing levels to meet acute inpatient care needs, which would result in APPs working 20% more weekends. Anticipation of this change in the setting of a 5-day workweek caused anticipatory stress related to burnout.
An annual institutional survey in 2021 reflected the national trend of increased burnout among health-care workers during the year 2020 (Maunder et al., 2022). This resulted in an expressed desire by the institution to support its employees with improved engagement and close examination of the processes that might change in order to mitigate the perception of burnout. As workplace flexibility is shown to be an integral part in reducing burnout among health-care workers, the authors sought to change the work schedule in order to improve job satisfaction (Sullivan et al., 2022). Concurrent departmental efforts to combat burnout included the establishment of a Wellness and Engagement Committee, which focused on organizing in-person social gatherings, employee appreciation initiatives, and compiling a wellness resources guide.
Implementation of a Condensed Workweek
The authors set out to reduce the occupational exhaustion component of burnout by adjusting the work schedule. It was felt that improvements in work-life balance with reduced occupational exhaustion would then improve employee engagement and a sense of personal accomplishment; to achieve this, the standard five 8-hour days per week would be changed to a condensed schedule of four 10-hour days.
As leadership buy-in is necessary for workflow shifts of this magnitude, it was important to reassure key stakeholders within the department that this process would not only benefit the APPs, but also the department and patient care. Interviews of managers within the institution who had successfully implemented a condensed APP work schedule confirmed that the transition was well-received and promoted a favorable work-life balance.
Initially, a formal presentation was given to departmental leadership involving an overview of a condensed workweek, a summary of successful institutional condensed workweek transitions, a detailed APP coverage plan of the proposed transition, and evidence of financial gain for the department in this scenario. After obtaining the approval of the departmental leadership, a schedule was created for the ID APPs. As there needed to be a minimum number of employees present to cover the clinical services, the weekdays that each person had off were staggered. These projections were based on the prior census coverage needs of the department. It was important that this change to the schedule would not affect patient care or productivity.
First, productivity data were collected from the inpatient ID services for the month preceding the new schedule. Ongoing data collection pre- and post-implementation was key in proving that this was a seamless transition. Updated details of the process were highlighted in regular one-to-one and monthly meetings for ID physicians, who were given opportunities to voice their concerns or provide constructive feedback during the process. The same information was shared during the monthly ID APP meetings, also with opportunities to provide feedback. This was particularly important in the initial 6-month pilot phase.
Assessment of Burnout and Work-Life Balance
A baseline assessment of the ID APPs’ level of burnout was conducted by issuing the Maslach Burnout Inventory along with additional questions about professional goals and overall job satisfaction for the ID APPs. Department physicians were also surveyed about their perceptions of the workflow of the inpatient services and any concerns they might have about a change in the APP schedule structure. The responses from the physicians indicated a slight apprehension that the change might affect patient care but showed their overall support to proceed with a trial schedule.
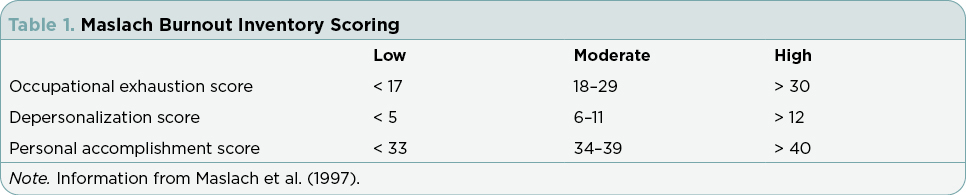
The Maslach Burnout Inventory measures three areas: occupational exhaustion, depersonalization or loss of empathy, and personal accomplishment. With occupational exhaustion, one shows a perception that work is difficult, tiring, or stressful. Unlike depression, it is likely to be improved by time away from work. Depersonalization or loss of empathy measures a loss of regard for others and emotional distancing, cynicism, and callousness. Personal accomplishment is a measure of fulfillment at work and a positive view of one’s professional achievements and is thought to act as a “safety valve” that can improve balance in the presence of increased occupational exhaustion or depersonalization (Table 1; Maslach et al., 1997).
Along with the Maslach Burnout Inventory, 10 additional ranked questions were asked to specifically assess the types of development projects with which the APPs at the institution are often engaged, and to assess baseline perceptions of work-life balance that could be followed during the trial (Table 2). This revealed APPs’ specific interests in educational, research, and quality improvement that they might be more likely to pursue with a different work schedule. Direct questions were asked on if they felt they were contributing in a meaningful way to the clinical team, and how they ranked their work-life balance.
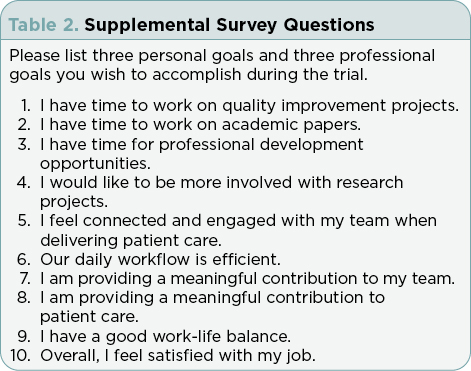
Open-ended questions about professional and personal goals that they hoped to achieve during the trial were asked. The personal goals were notably wholesome: to spend more quality time with family and friends, and to engage in personal fitness and other hobbies. The professional goals were varied, but with a majority expressing a desire to become more efficient at work, including prioritizing lunch breaks, followed by responses highlighting interests in teaching, writing manuscripts, and improving their own medical education.
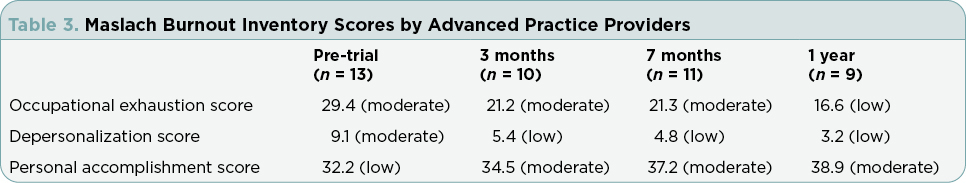
At the start of the trial, there were 15 APPs working in the ID department, and during this trial, the workforce increased to 17 APPs. The number of survey respondents varied from 9 to 13. The initial survey obtained prior to starting the new work schedule showed that the group as a whole had bordering high levels of occupational exhaustion, averaging at 29, with high levels starting at 30. There was a moderate level of depersonalization, and low levels of personal accomplishment. Subsequent surveys were given at 3 months, 7 months, and 1 year following the implementation of a condensed workweek. With each set of surveys, the group as a whole had exponentially improved scores in all three measures. At the 1-year survey, occupational exhaustion and depersonalization scored low, and personal accomplishment was moderate, but borderline to a high level (Table 3).
The supplemental questions directly assessing APPs’ perceptions of their ability to pursue professional goals, make meaningful contributions, and overall satisfaction with their jobs showed improvements. Prior to starting the trial, APPs reported moderate job satisfaction but low levels of work-life balance and a sense that they did not have time to work on professional goals. Over the course of the year with a condensed workweek, there was a great improvement of reports of overall job satisfaction, improved work-life balance, and achievement of personal and professional goals. There were still low to moderate levels of a sense that there is not enough time to work on professional goals, even though there were many accomplishments among the group. Professional projects that APPs worked on throughout the trial included giving lectures within the institution and at other institutions and at national conferences, precepting and mentoring physician assistant and nurse practitioner students, writing manuscripts for publication, conducting quality improvement projects for the institution, and participating in various institutional committees.
Conclusions
Advanced practice providers are crucial members of the health-care team. This article provides an overview of the successful implementation of a condensed workweek for ID APPs at a high-volume, high-acuity cancer center to counter burnout and health-care worker exhaustion. By implementing systemic workforce changes to the ID APP schedule, we measured quantifiable decreases in occupational exhaustion and depersonalization scores and increases in personal accomplishment scores via the Maslach Burnout Inventory over a 1-year period. This demonstrated that changes to workforce schedules improved employee satisfaction and mitigated burnout. Additional favorable outcomes of this process included a heightened ability to recruit and retain APPs and a significant fiscal gain, as the relative value units by the APP group increased by 4% in comparison with the prior year. Key factors ensuring seamless transition included key stakeholder buy-in, implementation of complex schedule solutions, and collaborative problem-solving for the team throughout the process.
Disclosure
The authors have no conflicts of interest to disclose.
References
American Association of Medical Colleges. (2021). The complexities of physician supply and demand: Projections from 2019 to 2034. https://www.aamc.org/media/54681/download?attachment
Barnell, C. (2023). 4-day workweek yields overwhelming success in U.K., researchers say. https://www.pbs.org/newshour/world/4-day-work-week-trial-yields-overwhelming-success-in-u-k-researchers-say
Kuriakose, C., Stringer, M., Ziegler, A., Hsieh, C., Atashroo, M., Hendershott, J.,…Mahoney, M. (2022). Optimizing care teams by leveraging advanced practice providers through strategic workforce planning. The Journal of Nursing Administration, 52(9), 474–478. https://doi.org/10.1097/NNA.0000000000001185
Maslach, C. (2017). Finding solutions to the problem of burnout. Consulting Psychology Journal: Practice and Research, 69(2), 143–152. https://psycnet.apa.org/doi/10.1037/cpb0000090
Maslach, C., Jackson, S. E., & Leiter, M. P. (1997). Maslach Burnout Inventory: Third edition.
Maunder, R. G., Heeney, N. D., Kiss, A., Hunter, J. J., Jeffs, L. P., Ginty, L.,...Wiesenfeld, L. A. (2021). Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors. General Hospital Psychiatry, 71, 88–94. https://doi.org/10.1016/j.genhosppsych.2021.04.012
Morgan, P. A., Smith, V. A., Berkowitz, T. S. Z., Edelman, D., Van Houtven, C. H., Woolson, S. L.,...Jackson, G. L. (2019). Impact of physicians, nurse practitioners, and physician assistants on utilization and costs for complex patients. Health Affairs (Project Hope), 38(6), 1028–1036. https://doi.org/10.1377/hlthaff.2019.00014
Sullivan, A. B., Davin, S. A., Lapin, B., Schuster, A. T., Dweik, R. A., Murray, K. F.,…Machado, A. G. (2022). Effects of flexible scheduling and virtual visits on burnout for clinicians. Multiple Sclerosis and Related Disorders, 60, 103705. https://doi.org/10.1016/j.msard.2022.103705
World Health Organization. (2019). Burn-out an “occupational phenomenon”: International Classification of Diseases. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases