Meeting Report
A Call to Action: The Role of the Oncology AP in Equitable Cancer Care
Brianna Hoffner,(1) MSN, ANP-BC, AOCNP®, Josh Epworth,(2) ARNP, Beth Faiman,(3) PhD, MSN, APRN-BC, AOCN®, FAAN, and Soumya J. Niranjan,(4) BPharm, MS, PhD
From (1)Harborside, Huntington, New York; (2)Seattle Cancer Care Alliance, University of Washington Medical Center, Seattle, Washington; (3)Cleveland Clinic Taussig Cancer Institute, Cleveland Ohio; (4)University of Alabama Birmingham
Presenters’ disclosures of conflicts of interest are found at the end of this article.
J Adv Pract Oncol 2022;13(3):213–216 |
https://doi.org/10.6004/jadpro.2022.13.3.6 |
© 2022 Harborside™

 ABSTRACT
ABSTRACT
The COVID-19 pandemic has only further brought to light how racism, bias, and lack of equity can result in social injustice, morbidity, and mortality. A panel of four advanced practitioners convened at JADPRO Live Virtual 2021 to examine oncology advanced practitioners’ capacity for enhancing equitable cancer care in the domains of care coordination and communication, clinical trials, and acknowledging and mitigating bias.
ARTICLE
In the spring of 2021, the Association of Community Cancer Centers (ACCC), Harborside, and collaborative partner Pfizer Oncology hosted a 3-day virtual summit to define the role of oncology advanced practitioners (APs) in equitable cancer care delivery. During JADPRO Live Virtual 2021, Brianna Hoffner, MSN, ANP-BC, AOCNP®, Josh Epworth, ARNP, Beth Faiman, PhD, MSN, APRN-BC, AOCN®, FAAN, and Soumya J. Niranjan, BPharm, MS, PhD, expanded upon this conversation with a panel discussion about equitable and inclusive cancer care.
The presenters described how implicit and explicit bias affect cancer care and influence outcomes, identified tools to assess bias at both personal and institutional levels, discussed the importance of supporting cancer research, and reiterated the role of the oncology AP in advancing equitable cancer care delivery.
“Over the past year and a half of the COVID-19 pandemic, we have seen how racism, bias, both implicit and explicit, and lack of equity can result in social injustice, morbidity, and mortality,” said Ms. Hoffner, Director of Clinical Outreach and Development at Harborside. “All members of health-care teams across the country have grappled with the reality that quality care is equitable care, but we are far from achieving this future state. However, oncology advanced practitioners are uniquely positioned to effect change.”
Coordination and Communication in Cancer Care
As Mr. Epworth explained, care coordination is the deliberate organization of patient care activities between two or more participants (including the patient) involved in the patient’s care to facilitate the appropriate delivery of health-care services. The absence of good care and coordination results in several negative outcomes, including poor symptom control, medical errors, greater utilization of the emergency department, increased costs, decreased patient satisfaction, and poor follow-up.
“Thankfully, we have a growing number of resources at our disposal as we have begun to recognize the importance of care coordination,” said Mr. Epworth.
These resources include nurse navigators, clinical care coordinators, and social workers as well as new developments such as the multidisciplinary care team and meeting planning. Telehealth, telemonitoring, and global access to electronic medical records (EMR) are additional tools that have seen increased use because of the COVID-19 pandemic, and these tools can improve access to clinical trials, supportive care, and survivorship care. Partnerships with local clinics can also be an important asset to coordinating care.
Despite these new assets, however, Mr. Epworth noted a multitude of barriers to coordinating care that change depending on the group, individual, and health-care situation. These barriers include financial toxicity, low health literacy, and mistrust between facility and patient.
“We have groups in this country that have had a very negative experience with the medical system, and we have some people who have developed mistrust personally of the medical system either from what they have read somewhere or a negative interaction with a medical care facility,” said Mr. Epworth.
Another issue that can impact the coordination of care is restrictive access to secondary coverage. Coordinating care while managing insurance needs can be a significant use of time, said Mr. Epworth.
Although there has been a boom in the use of telemedicine, Mr. Epworth also noted that not every part of the country has access to high-speed internet, especially in rural parts of the country, and there are language and cultural barriers that can impede coordination in the clinic, too.
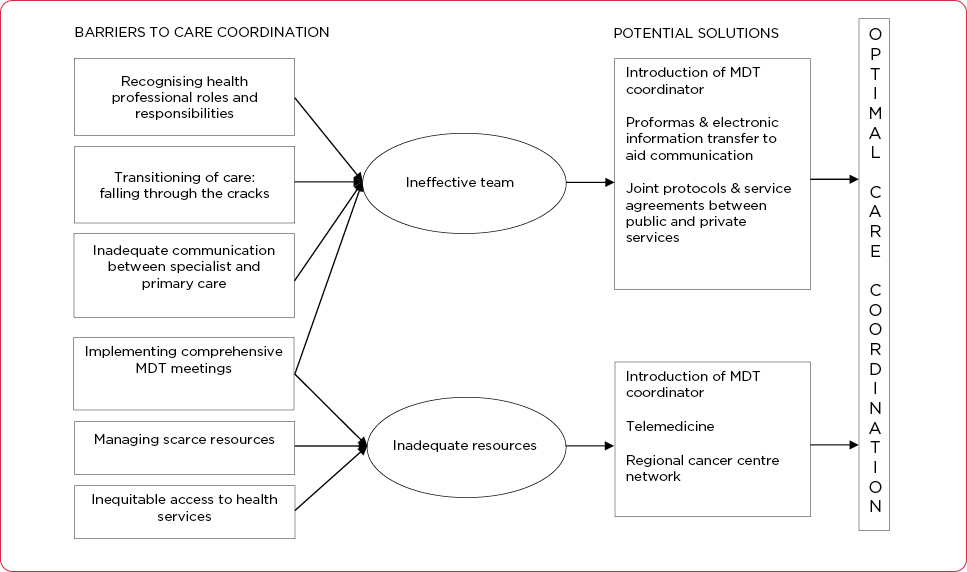
A recent qualitative study that identified several barriers to coordination of cancer care also proposed potential solutions (Walsh et al., 2010). These include the introduction of a multidisciplinary team coordinator, proformas and electronic information transfer to aid communication, and service agreements between public and private services. The researchers also promoted increased use of telemedicine if available and regional care networks to improve communication and access to care (Figure 1).
“The first step needed for change is recognizing that as providers and as institutions we may have blind spots regarding the complexities of coordination,” said Mr. Epworth.
“Once we’ve identified barriers to coordination and acknowledged how they impact our patients, we can develop mechanisms that can bridge coordination shortfalls, whether it’s with a patient, the patient’s family, the primary caregiver, or their community clinic,” he continued. “Finally, like all good research, we must assess and re-assess our approach as times change.”
Equity in Clinical Trial Design, Conduct, and Engagement
According to Dr. Faiman, a nurse practitioner at the Cleveland Clinic Taussig Cancer Institute in Ohio, the pandemic has allowed more clinical trial participation and changed clinical trial conduct to be more inclusive, but there is still work to be done.
“Clinical trials are critical to test new methods of screening, prevention, diagnosis, and treatment of a condition,” she explained. “Unfortunately, although trials are designed to be representative of a population study to produce clinically meaningful outcomes for patients, ethnic, cultural, socioeconomic, and other minorities are excluded from clinical trials all too often.”
Dr. Faiman underscored the importance of oncology APs to equity in design, recruitment, and clinical trial completion. A single or cumulative voice of oncology APs can highlight issues with the design of clinical trials and can enhance diversity.
Other important issues include patient and clinician education, knowledge of barriers, and institutional support. For example, said Dr. Faiman, researchers can consider various trial design and methodologic issues that will allow cancer patients to participate, such as opening the clinical trial in the community for patients unwilling or unable to travel downtown.
“We really need different ethnic minorities,” she said. “It is essential to identify differences in pharmacokinetic efficacy and the safety of these groups in a subpopulation.”
Another key issue in clinical trial conduct and engagement is the measurement of equity in clinical trials (or error). As Dr. Faiman explained, equity in health refers to absence of unnecessary or avoidable differences in health that are considered unfair and unjust. Populations that experience disadvantages or opportunities that are lacking can lead to poor health outcomes, she said.
There are also disparities in clinical trial design. While simple demographics, such as age, gender, and race, are often collected during the context of clinical trials, said Dr. Faiman, few studies specifically collect how many patients are LGBTQ.
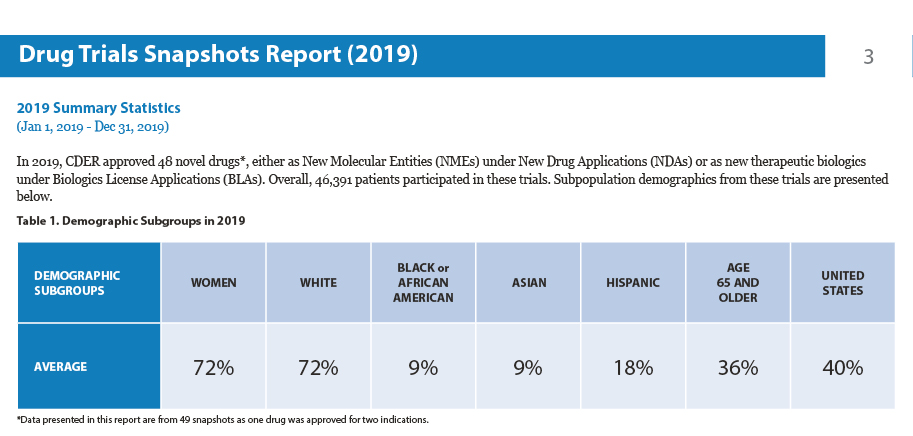
Finally, equity in clinical trials can be hindered by recruitment challenges and patient participation, which may arise from lack of trust in the provider health-care system (Figure 2).
“It’s been said that the process and methodology of a well-designed clinical trial is just as important as the results,” Dr. Faiman concluded. “I also feel that everyone should have the opportunity to participate in a well-designed clinical trial, regardless of race, gender, or culture.”
Implicit Bias in Cancer Care and Outcomes
Dr. Niranjan, an assistant professor at the University of Alabama Birmingham, said that the term “bias” is not just about explicit prejudice but also refers to implicit stereotypes that can be seen between patient-provider interactions that may affect treatment decisions, treatment adherence, and patient health outcomes.
“While psychologists often define bias broadly, such as ‘the negative evaluation of one group and its members relative to another,’ it’s important to note what happens after that negative evaluation,” said Dr. Niranjan, who reported that health-care professionals have been shown to exhibit the same levels of implicit bias as the wider population.
According to Dr. Niranjan, there are plenty of biases that providers need to be cognizant of, but cancer type and racial bias are two important forms. In a recent study, members of professional gynecology/oncology organizations were asked to complete two Implicit Association Tests to determine if they implicitly associate cervical cancer with feelings of anger (prejudice) and beliefs about culpability for the disease (stereotypes), compared with ovarian cancer (Liang et al., 2019). Results of the study found significant levels of implicit bias related to cervical cancer among gynecology oncology providers, including both prejudice and stereotyping.
With respect to racial bias, Dr. Niranjan noted that implicit racial bias is negatively associated with oncologist communication, patients’ reactions to racially discordant oncology interactions, and patient perceptions of recommended treatments. A recent study of bias and stereotyping among research and clinical professionals, for example, found that some respondents viewed racial and ethnic minorities as less-promising participants and reported withholding trial opportunities from minorities based on these perceptions (Niranjan et al., 2020).
“We must all advocate for zero tolerance for delivering substandard care, and we have an obligation to correct these discrepancies,” said Dr. Niranjan. “It’s not about saying that one is biased over the other; it is about moving forward and trying to correct them. We must all figure out our own ways of fighting for our patients to receive the best possible care.”
According to Dr. Niranjan, this means making sure that people who are seen in community practices have opportunities to participate in clinical trials. When there are opportunities to participate, she said, providers must ensure that people are offered, and most importantly, that people are aware so that they can take advantage of these opportunities.
Disclosure
Mr. Epworth, Ms. Hoffner, and Dr. Niranjan had no conflicts of interest to disclose. Dr. Faiman has served on advisory panels for Celgene, GlaxoSmithKline, Karyopharm, and Sanofi Genzyme.
References
Liang, J., Wolsiefer, K., Zestcott, C. A., Chase, D., & Stone, J. (2019). Implicit bias toward cervical cancer: Provider and training differences. Gynecologic Oncology, 153(1), 80–86. https://doi.org/10.1016/j.ygyno.2019.01.013
Niranjan, S. J., Martin, M. Y., Fouad, M. N., Vickers, S. M., Wenzel, J. A., Cook, E. D.,…Durant, R. W. (2020). Bias and stereotyping among research and clinical professionals: Perspectives on minority recruitment for oncology clinical trials. Cancer, 126(9), 1958–1968. https://doi.org/10.1002/cncr.32755
Walsh, J., Harrison, J. D., Young, J. M., Butow, P. N., Solomon, M. J., & Masya, L. (2010). What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Services Research, 10, 132. https://doi.org/10.1186/1472-6963-10-132