Grand Rounds
Thrombocytopenia, Deep-Vein Thrombosis, and Pulmonary Emboli in a Patient With Primary CNS Lymphoma
Patricia Palmer, RN, MS, AOCNS®
From University of California, Davis Health System, Sacramento, California
The author has no conflicts of interest to disclose.
Correspondence to: Patricia Palmer, RN, MS, AOCNS®, University of California, Davis Health System, Nursing Administration, 2315 Stockton Blvd, Sacramento, CA 95817. E-mail: patricia.palmer@ucdmc.ucdavis.edu
J Adv Pract Oncol 2011;2:112–121 |
DOI: 10.6004/jadpro.2011.2.2.5 |
© 2011 Harborside Press®
 ABSTRACT
ABSTRACT
Case Study
M.F. is a 64-year-old male who presented to an outside hospital in May 2003 with chief complaints of headache, confusion, facial edema, and dysphasia. A magnetic resonance imaging (MRI) scan revealed a left frontal lobe mass. The pertinent past medical history included localized prostate cancer diagnosed 3 years prior, which was confined to the prostate and had been treated surgically. The patient also had a history of partial colectomy for a benign colonic condition 3 years prior and a history of gastroesphogeal reflux disorder. M.F. was transferred to the University Hospital, and on May 10 he had a brain biopsy and subtotal tumor resection of a deep frontal lobe mass. The biopsy was positive for a diffuse large B-cell non-Hodgkin lymphoma (NHL). A staging workup including computed tomography (CT); scans of the chest, abdomen, and pelvis and bilateral bone marrow biopsies were negative, and the diagnosis was confirmed as primary central nervous system lymphoma (PCNSL).
The patient was started on high-dose methotrexate (8 g/m2 every 2 weeks) on May 19. On May 20 he had a single-lumen venous access port (VAP) placed. He had a rapid improvement in his memory, vocal strength, and energy. On June 17 M.F. presented for his third cycle of methotrexate; his platelet count, which had been 195,000/μL at the start of chemotherapy on May 19, was now 88,000/μL. A peripheral smear was reviewed which showed no platelet clumping, and the patient's platelet count remained in the 80,000/μL
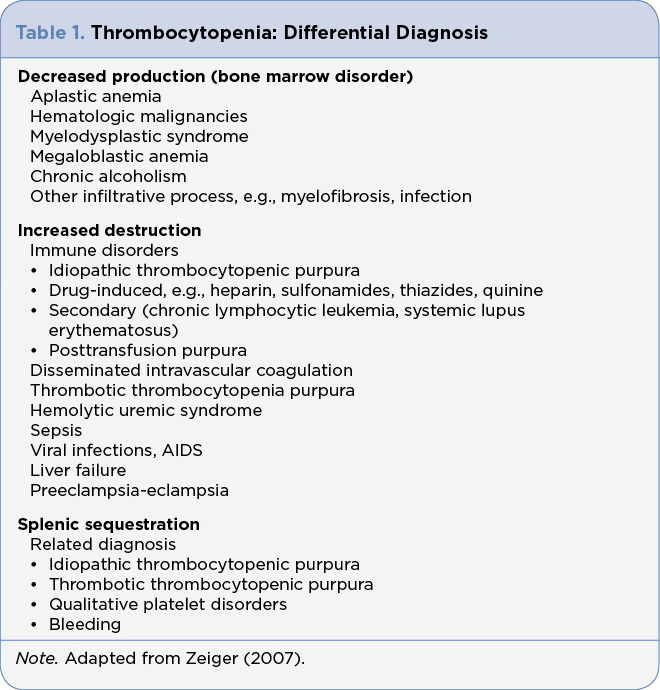
range during his 5-day hospitalization. It was decided to get a 1-week count in follow-up when the patient presented to the outpatient infusion room for his weekly VAP flush of 3 mL of 1:100 unfractionated heparin (UFH). The repeat platelet count was 134,000/μL. When the patient presented for cycle 4 of methotrexate on June 30 his platelet count was 114,000/μL and it dropped to 96,000/ during the hospitalization. The differential diagnosis for thrombocytopenia included disorders of decreased production, increased destruction, and splenic sequestration (Zeiger, 2007; Table 1).
M.F. was on a leucovorin calcium rescue (100 mg/m2 every 6 hours) to prevent side effects from the chemotherapy. His medications were oral dexamethasone, which was being tapered (currently 4 mg daily), and oral rabeprazole (Aciphex) 20 mg daily. He was completely asymptomatic and had no evidence of bleeding or bruising. He reported mild bilateral lower extremity edema. A heparin-induced thrombocytopenia (HIT) enzyme-linked immunosorbent (ELISA) assay was drawn, as well as a Factor V mutation; his port was flushed with normal saline while the lab results were awaited.
M.F. returned for his fifth cycle of high-dose methotrexate on July 15. His platelet count on admission was 190,000/μL. He now complained of a fever of 102°F (at home) that he felt was due to a spider bite on his ear. On admission, he had the following: temperature 38.4°C, pulse 80, blood pressure 109/63, 18 respirations/min, and oxygen saturation (O2) 96% on room air. The patient's absolute neutrophil count was 3,150/μL. Cultures were drawn and it was decided to proceed with the planned chemotherapy because the patient was not neutropenic.
During the night of the first day of admission M.F. spiked a temperature of 39.4°C. His O2 saturation dropped to 80% but improved to 96% with movement and deep breaths. He was briefly placed on O2 per nasal cannula at 2.0 L. M.F. was sitting up in a chair, dressed, completely asymptomatic, and without O2 on exam the next morning. Specifically, he denied chest pain or shortness of breath, the spider bite on his ear was not secondarily infected, and he had some areas of white patches on his tongue. A spiral CT was ordered and the patient was found to have bilateral acute pulmonary emboli in the left lower lobe and right middle lobe. A Doppler study on his lower extremities showed an acute non-occluding deep-vein thrombosis (DVT) in the right popliteal vein extending into the trunk. His Factor V Leiden test was negative as was his ELISA assay for HIT. The comment on the test result suggested that if there were clinical evidence of HIT (i.e., thrombocytopenia at least 50% lower than baseline), alternative tests should be considered. A Serotonin Release Assay was ordered but it was cancelled because the send-out test was not available. The patient was placed on lepirudin, a heparin allergy was placed on his chart, and he was eventually switched to warfarin sodium upon discharge home.
For access to the full length article, please
sign in.